Cancer ravages both body and mind. If you’ve ever lost loved ones to the disease, you might recognize the physical and emotional changes cancer patients often endure during their final months. They seem drained of strength and spirit. Even people who’ve maintained a positive outlook throughout their lives can enter a state of despair. New research published in Science suggests apathy and lack of motivation are symptoms of a condition called cancer cachexia. Cold Spring Harbor Laboratory (CSHL) Associate Professor Tobias Janowitz explains:
“Many patients complain of symptoms in that category. They say, ‘I don’t know what’s going on with me. My relatives cooked my favorite meal. I don’t feel like eating it.’ Their grandchildren come for a playdate. Usually, they’d be excited and enjoy it. They just don’t seem to engage so much.”
Also frustrating, cachexia severely limits patients’ ability to tolerate common cancer treatments. CSHL scientists have been studying the condition for years. Now, in a major development, Janowitz and colleague Adam Kepecs at Washington University School of Medicine in St. Louis (WashU Medicine) have identified a connection between the brain and the immune system that is responsible for cachexia-related apathy.
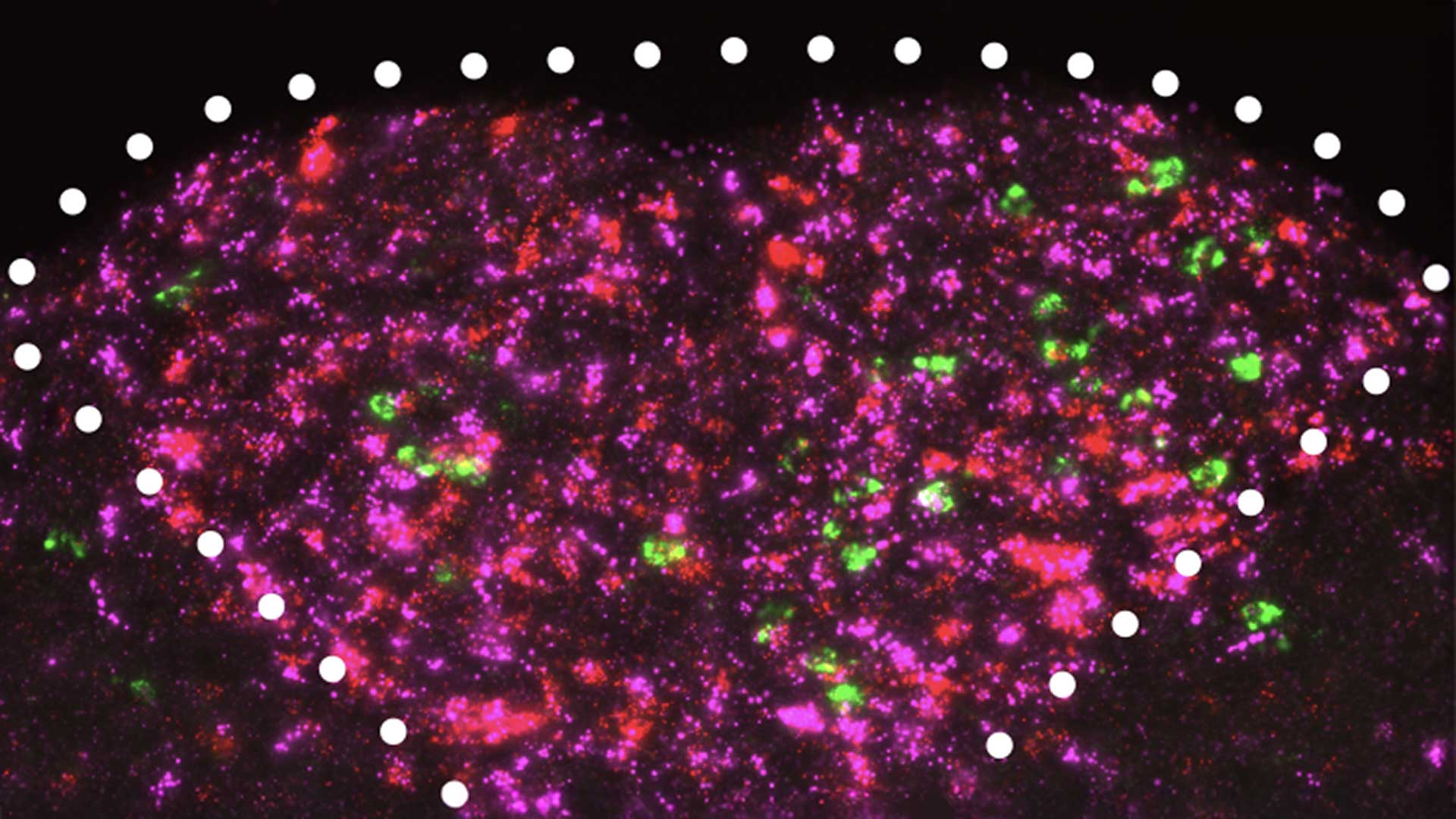
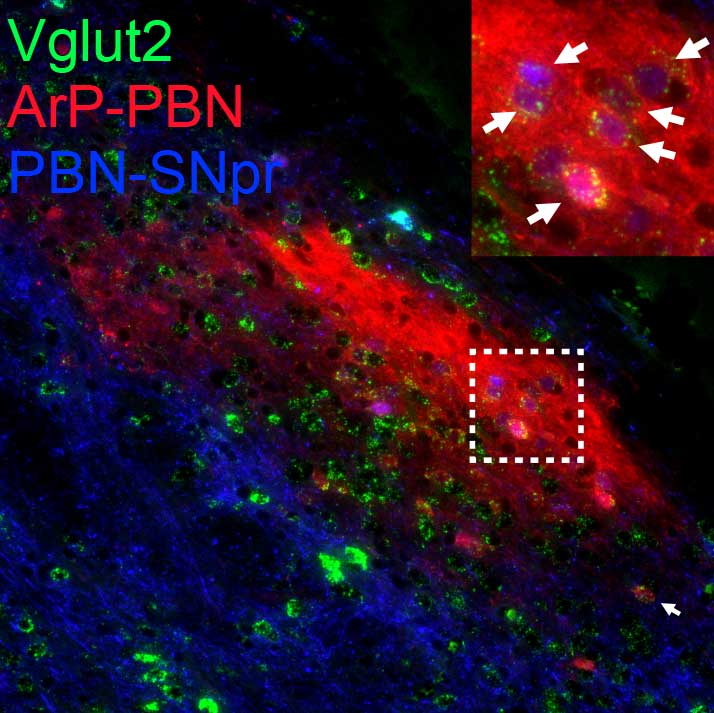
They found that as cachexia progresses, certain neurons release less and less dopamine. That’s the brain’s “feel-good” chemical. Screening for elevated immune system proteins in the brains and bodies of mice with cachexia led the team to IL-6, which gets released during inflammation and has long been associated with cachexia. Decreasing IL-6 signals in connected brain areas made the mice more motivated. Notably, the mice became less sensitive to the amount of effort required to find food. The scientists saw the same result when elevating dopamine levels in the right brain areas.
“We discovered a full brain circuit that senses inflammation in the bloodstream and sends signals that reduce motivation,” Kepecs says. “This reveals that apathy isn’t just an emotional or psychological reaction to cachexia—it’s built into the biology of the disease.”
The discovery further suggests that existing antibody treatments could be repurposed to improve cancer patients’ quality of life. “Our goals are to make patients feel better and to treat the cancer better,” Janowitz explains.
“A better patient will be able to better tolerate and benefit from anti-cancer treatments.”
Working across cancer and neuroscience has brought the researchers this far. Their ultimate hope is that one day, through continued interdisciplinary collaboration, they will help turn cachexia into a condition patients can overcome. That would be a welcome development not only for people battling cancer but also for their loved ones who suffer alongside them.
Written by: Jennifer Michalowski, Science Writer | [email protected] | 516-367-8455
Funding
National Institute of Child Health and Human Development, German Research Foundation, La Caixa Foundation, The Mark Foundation for Cancer Research, Cancer Grand Challenges, Taylor Family Institute for Psychiatric Research, Hope Center for Neurological Disorders, McDonnell Center for Systems Neuroscience, The Brain & Behavior Research Foundation
Citation
Zhu, X.A., et al., “A neuro-immune circuit mediates cancer cachexia-associated apathy”, Science, April 11, 2025. DOI: 10.1126/science.adm8857
Core Facilites
Principal Investigator

Tobias Janowitz
Associate Professor
Cancer Center Program Co-Leader
M.D., Ph.D., University of Cambridge, UK, 2007