Cold Spring Harbor Laboratory (CSHL) Professor Hiro Furukawa takes an architectural approach to brain research. He creates structural 3D maps of important proteins that malfunction in brain disorders. Furukawa has zeroed in on a protein called the NMDA (for N-methyl-D-aspartate) receptor that plays a key role in learning and memory. The NMDA receptor acts as a channel to allow ions into neurons to activate them. When the NMDA receptor doesn’t work properly, neurons can fire at the wrong times, which can result in disorders like Alzheimer’s disease, depression, and epilepsy.
The Furukawa lab’s maps provide a unique, atomic point of view of the NMDA receptor. They let his team look, in 3D, at how the protein’s atoms are arranged and move. Knowing the precise details of NMDA’s structure allows scientists to develop and optimize therapeutics from new angles.
“We’re trying to essentially provide a blueprint for optimizing drugs that have the potential to treat disorders but [currently] cause dangerous side effects,” Furukawa says. Drugs that fit and match up perfectly to the NMDA receptor or channel could have more benefits and fewer side effects.
Using these maps, Furukawa and his team have innovated two new routes for optimizing NMDA therapeutics. One is to pinpoint the perfect spot where drugs should bind to minimize side effects. Their second approach looks at how well drugs bind to the NMDA channel to maximize their impact.
Picking your battles
Most drugs for neurological disorders like Alzheimer’s suffer from severe side effects because they don’t fit just right. They don’t bind well enough to the NMDA receptor and set off unwanted reactions. Furukawa and his team recently used their detailed maps of the NMDA receptor structure to design a molecule that fits perfectly.
The team developed antibodies, or “picky proteins,” that may avoid unwanted side effects by being very picky about what they target. It is designed to bind to a specific spot on the NMDA receptor. When the picky protein binds, it restricts the receptor’s movement and helps close its ion channel. This prevents too many ions from getting through and neurons from activating at the wrong times.
This video shows the antibody, a “picky protein,” developed by the Furukawa lab latching onto the top of the NMDA receptor and preventing neurons from being overactive.
Furukawa and his team are now optimizing the design of the picky protein to improve its potential and efficacy for clinical use. Their work was published in the journal Nature Communications.
While pinpointing the perfect spot for a drug to bind has its advantages, drugs must also stay bound long enough to have a beneficial effect. Furukawa and his team leveraged their blueprints to explore this second route for optimizing therapeutics using three psychotropic drugs. These drugs affect behavior, mood, thoughts, or perception.
Paying attention to detail
In the journal Nature Structural and Molecular Biology, Furukawa and his colleagues published a study where they created maps of different drugs bound to the NMDA receptor channel. This let them figure out how long the drugs were able to stick and block the flow of ions. The longer they stayed connected, the greater the potential beneficial effect for treating neurological disorders.
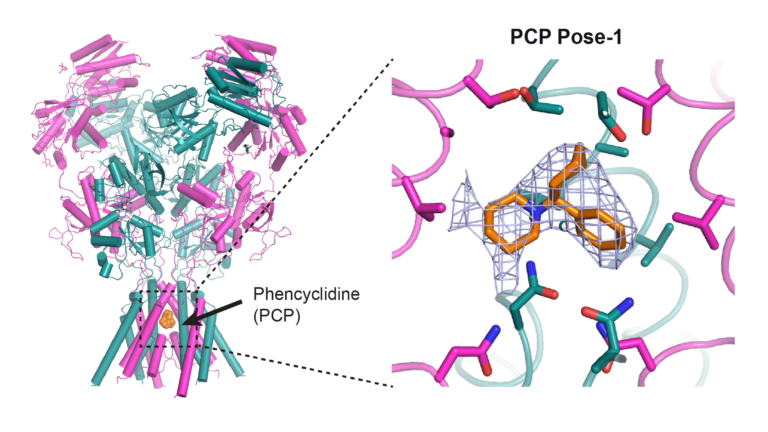
The team looked at the binding properties of two FDA-approved drugs, ketamine and memantine. In an unconventional move, they also looked at the recreational drug PCP. Developed in 1959, PCP can cause hallucinations and symptoms akin to schizophrenia. With the help of their atomic maps, the team showed that PCP remained attached the longest. It also blocked the function of the NMDA receptor the best, followed by ketamine and memantine. “This may explain why PCP has more robust psychotic side effects than the other drugs,” says Furukawa.
The team is working on understanding what allows PCP and the other drugs to bind differently. This may help guide the development and improvement of therapeutics to treat brain disorders.
Better therapeutics
The Furukawa lab is continuing to dive deeper into the architecture of NMDA receptors. At this time, they are working to zoom in even closer and bring greater detail to their atomic blueprints. Higher-resolution maps may help reveal new angles to improve current and future therapeutics.
Although Furukawa and his team are focused on the small details of the NMDA receptor, he hopes his work has a much bigger, long-term impact on brain health. “Currently available drugs for Alzheimer’s disease are only effective for a short period of time,” he says. “We want to help to develop reagents that boost cognition for a longer period of time in the order of multiple years.”
Written by: Daniel Dunaief, Science Writer | publicaffairs@cshl.edu | 516-367-8455
About
Hiro Furukawa
Professor
Ph.D., The University of Tokyo, 2001
