Research reveals a mechanism that causes wasting in cancer and tests a way to reverse it
Cold Spring Harbor, NY — One of the worst cruelties of lethal cancer is the phenomenon called wasting, or in medical terms, cachexia (pronounced ka-CHEX-ia), in which a patient seems literally to diminish in bodily terms as the cancer ravages one or more internal organs.
Today, a team at Cancer Research UK Cambridge Institute, led by Professor Douglas Fearon, M.D., of Cold Spring Harbor Laboratory in New York and a Distinguished Scholar of the Lustgarten Foundation, publishes in Cell Metabolism results of experiments showing that tumors interfere with the patient’s ability to cope with wasting and may even impair their ability to respond to immunotherapy.
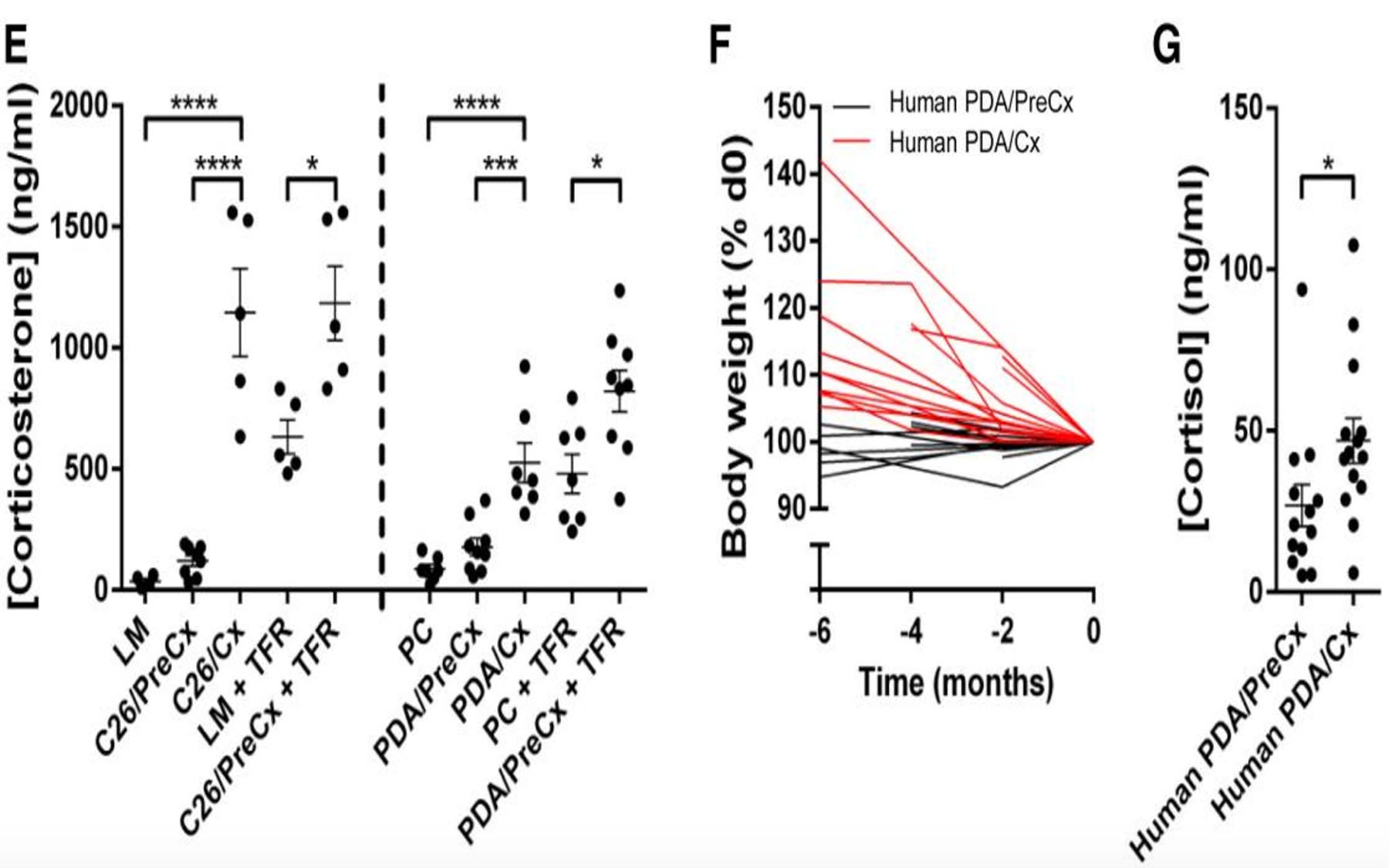
In mouse models of human pancreatic and colon cancer, the team traces cachexia to a molecular reprogramming of the liver induced by the tumor, the effect of which is to alter the liver’s normal response to caloric deficiency. As the caloric deficiency worsens and weight continues to decline, the body responds by releasing stress hormones. The team found that these hormones, in turn, prevent the immune system from responding to the tumor.
The tumor reprograms liver metabolism, altering the organ’s normal response to caloric deficiency. As wasting takes hold, the body responds by releasing stress hormones, which in turn prevent the patient’s immune system from responding to the tumor.
Thus the new research helps explain two ways in which pancreatic and colon tumors have long vexed doctors attempting to treat them: these tumors themselves set in motion the process that results in wasting; and wasting, in turn, accounts for why immune therapy for such cancers has typically failed. Providing massive caloric supplementation—what doctors call hyperalimentation—does not vanquish wasting; and immune therapy does not impair the tumor’s ability to thrive.
The researchers in Cambridge, led by M.D.-Ph.D. student Thomas R. Flint and oncologist Tobias Janowitz, M.D., Ph.D., performed experiments demonstrating that in mouse models of pancreas and colon cancer, liver reprogramming begins during pre-cachexia, when wasting has just begun but is not yet manifest. Signals broadcast by tumor cells induce the release of interleukin 6 (IL-6), a molecular beacon of the immune system called a cytokine, that normally helps induce an immune response. IL-6, in turn, impairs the capacity of the liver to respond to caloric deprivation, which is already underway in pre-cachectic mice.
The team proposes this liver reprogramming is the result of IL-6 suppressing a gene-regulating protein, or transcription factor, called PPAR-alpha, which in turn suppresses a vital process in the liver called ketogenesis. “Translated into human terms, this means that when a cancer patient loses his or her appetite and decides not to eat, the liver is not going to generate sufficient energy to compensate for the caloric loss,” explains Dr. Fearon.
Often, cancer patients don’t eat, Dr. Fearon clarifies, not because they are nauseous due to chemotherapy; rather, they feel full and simply lose their appetite. Importantly, he adds, his team’s discovery that the tumor is programming the liver not to make calories, which are essential for continued brain function, assures two things. One is that wasting will continue; the other is that the body, massively releasing glucocorticoids, or stress hormones, will thereby short-circuit the immune system’s ability to respond to the tumor. It’s a vicious circle that sadly ends in death.
The team’s discovery not only sheds light on why conventional caloric supplementation fails to curtail cachexia in cancer patients. It also helps to account for the failure of T-cell checkpoint targeted immunotherapies in pancreatic and colon cancers. The tumor, in effect, is fooling the immune system into thinking the tumor is not a threat but rather just normal regenerating tissue.
Successful reversal of cachexia may depend on co-administration of an antibody that inactivates IL-6 and nutritional support.
The team tested several ways of addressing liver reprogramming in pre-cachectic mice. Using a mouse model that recapitulates human pancreatic cancer, they administered an antibody that targets and inactivates IL-6; the same mice received massive caloric supplements via infusion. According to Dr. Flint, “Our data suggest that successful reversal of cachexia in people may well depend on co-administration of anti-IL-6 with nutritional support.”
The team also noted that their findings may have relevance in a wide range of IL-6-associated illnesses in which weight loss in observed. These include sepsis, HIV, tuberculosis, chronic obstructive pulmonary disease, cardiac failure and rheumatoid arthritis.
Written by: Peter Tarr, Senior Science Writer | publicaffairs@cshl.edu | 516-367-8455
Funding
The research described here was supported by: The Lustgarten Foundation for Pancreatic Cancer Research; Cancer Research UK; The Ludwig Institute for Cancer Research; the NIHR Biomedical Research Centre and the Cambridge ECMC.
Citation
“Tumor-induced IL-6 reprograms host metabolism to suppress anti-tumor immunity” appears November 8, 2016 in Cell Metabolism. The authors are: Thomas R. Flint, Tobias Janowitz, Claire M. Connell, Edward W. Roberts, Alice E. Denton, Anthony P. Coll, Duncan I. Jodrell and Douglas T. Fearon. The paper can be viewed at: http://www.cell.com/cell-metabolism/home
The Lustgarten Foundation
The Lustgarten Foundation is the largest private foundation dedicated to funding pancreatic cancer research. The Foundation supports research to find a cure for pancreatic cancer, facilitates dialogue within the medical and scientific community, and educates the public about the disease through awareness campaigns and fundraising events. Since its inception, the Foundation has directed more than $125 million to research and assembled the best scientific minds with the hope that one day, a cure can be found. Thanks to private funding, 100 percent of every dollar donated to the Foundation goes directly to pancreatic cancer research. For additional information, please visit www.lustgarten.org.
Principal Investigator

Douglas Fearon
Professor
Cancer Center Member
M.D., Johns Hopkins University School of Medicine, 1968